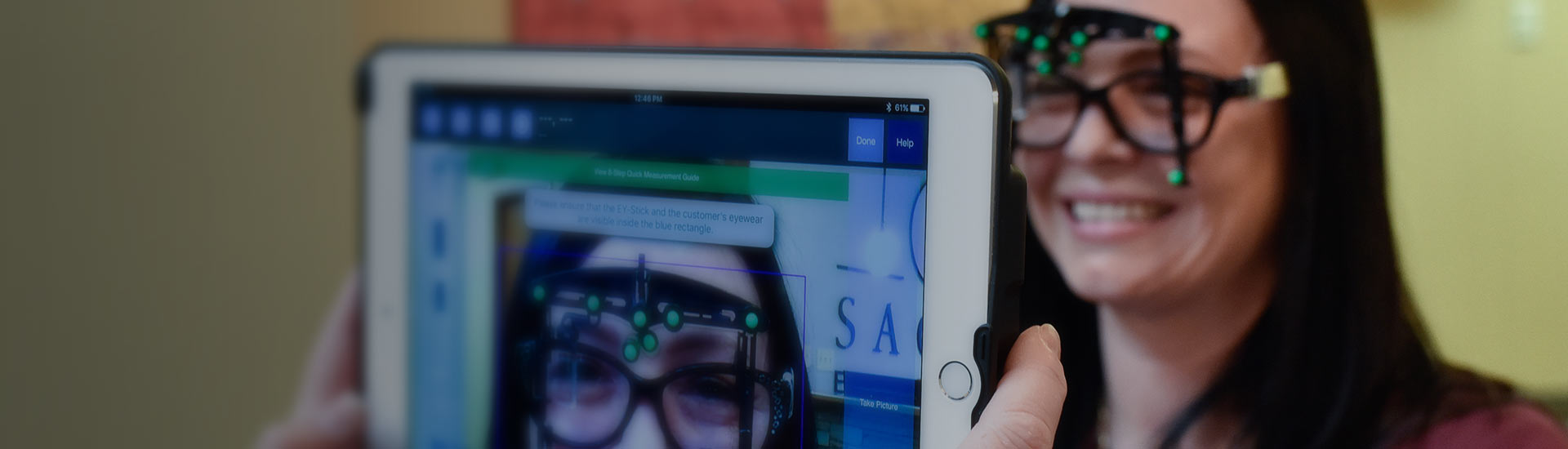
Our Practice
Enhancing the lives of the people we touch on a daily basis.

Patient Portal
Your records, prescriptions, information and correspondence at your fingertips.

Order Contact Lenses
Your contact lens prescription can be filled here and delivered right to your door.

Contact Us
Office hours, directions and documents.
Email us here or request an appointment.
Email us here or request an appointment.